Joint Replacement
Joint replacement surgery is a highly effective treatment for patients with severe joint damage, most often caused by arthritis, injury, or long-term wear and tear. The procedure involves replacing the damaged joint surfaces with artificial implants, relieving pain, restoring mobility, and improving quality of life.
This page explains the different types of joint replacement surgery in the UK, when it is recommended, what the procedure involves, and what to expect during recovery.
What is Joint Replacement Surgery?
A joint replacement (also called an arthroplasty) is a surgical procedure in which the worn or damaged surfaces of a joint are removed and replaced with prosthetic components made of metal, ceramic, or plastic.
The most common joint replacements are:
- Hip replacement
- Knee replacement (total or partial)
Conditions Treated with Joint Replacement
Joint replacement may be recommended for patients with:
- Severe osteoarthritis
- Rheumatoid arthritis
- Avascular necrosis (AVN) of the hip
- Post-traumatic arthritis following injury
- Failed previous surgery or joint deformities
Benefits of Joint Replacement Surgery
Joint replacement can provide significant improvements, including:
- Pain relief
- Improved mobility and stability
- Correction of deformities
- Better quality of life
- Return to daily activities and low-impact sport
Types of Joint Replacement
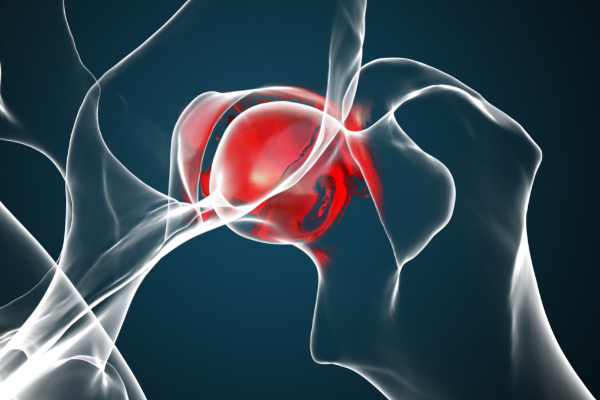
Hip Replacement
- Damaged hip joint replaced with a prosthetic ball and socket
- Can be performed as a total hip replacement or partial hip replacement
- Often carried out as a day case procedure in the UK
Knee Replacement
- Options include total knee replacement (all compartments replaced) or partial knee replacement (only damaged areas treated)
- Robotic-assisted techniques may improve accuracy and recovery times
The Joint Replacement Procedure
Before
- Assessment with X-rays and scans
- Pre-operative physiotherapy and planning
- Discussion of risks, benefits, and implant choices
During
- Performed under a general or spinal anaesthetic
- Damaged joint surfaces removed and replaced with implants
- Procedure length: usually 1–2 hours
After
- Early mobilisation encouraged (sometimes the same day)
- Hospital stay of 1–2 nights for many patients
- Physiotherapy begins immediately to support recovery
Recovery After Joint Replacement
Short-Term Recovery
- Walking aids (crutches or frame) used initially
- Most patients return home within a few days
- Swelling and discomfort managed with medication and physiotherapy
Rehabilitation Timeline
- 0–6 weeks: Walking with support, gentle exercises
- 6–12 weeks: Increased strength and mobility
- 3–6 months: Return to normal daily activities
- 6–12 months: Full recovery for most patients

Risks and Complications
Joint replacement is a safe and routine procedure in the UK, but possible risks include:
- Infection
- Blood clots
- Stiffness or reduced mobility
- Implant loosening or wear over time
- Rare need for revision surgery
Why Choose Mr Mark Webb for Joint Replacement
When you choose Mr Mark Webb for your joint replacement surgery, you can expect:
-
A comprehensive, accurate diagnosis using modern imaging and assessment tools to understand exactly which joint(s) are damaged and how
-
A personalised surgical plan tailored to your health, anatomy, lifestyle and goals, including whether a partial or total replacement is best for you
-
Access to high quality implants (metal, ceramic, polyethylene, etc.) and advanced surgical techniques—including minimally invasive or robotic-assisted options where appropriate—to maximise function and durability
-
A structured rehabilitation programme to support your recovery, regain strength and mobility, and reduce complications
-
The best chance of reducing pain, restoring joint function, improving quality of life, and maintaining long-term joint health
Frequently Asked Questions
How do I know if I need a joint replacement?
You might need joint replacement if you have joint pain or stiffness that has not responded to non-surgical treatments (e.g., medication, physiotherapy, injections), if your pain significantly limits your daily activities or quality of life, or if imaging (X-ray, MRI) shows advanced joint damage.
What joints can be replaced, and what are the options?
Common joints replaced include the hip and knee, but replacements are also possible in other joints (shoulder, ankle) depending on damage. Options include total replacement (replacing the damaged joint surfaces fully) or partial replacement (only replacing part of the joint if only that portion is worn or damaged).
What benefits should I expect after joint replacement?
After a successful joint replacement, many people report dramatic pain relief, improved mobility and ability to perform daily tasks, better quality of life, and increased independence. Modern implants are durable, and many people enjoy years of function from their new joint.
What is recovery like, and how long will it take to get back to my normal life?
Recovery depends on which joint is replaced, how healthy you are beforehand, and how closely you follow rehab. Early steps include pain control, wound care, and beginning physical therapy. Some people are able to walk with assistance soon after surgery. Everyday activities often improve significantly by 4-6 weeks; full recovery may take several months up to a year.
What are the risks or complications of joint replacement?
Joint replacement is generally safe, but like any major surgery, there are risks. These include infection, blood clots, implant wear or loosening over time, stiffness, and sometimes ongoing pain. Certain patient factors—such as age, general health, co-existing conditions—can affect risk. Discussing these with your surgeon helps you understand what you can do to reduce risk.

